This post may contain affiliate links. If you click through a link and make a purchase, I may receive a commission at no additional cost to you. As an Amazon Associate, I earn from qualifying purchases. Read the full disclosure here.
Few things are more frustrating than wasting time on treatments that don’t work.
Piriformis syndrome and sciatica can present with similar symptoms, however, their underlying causes are different and therefore respond to different treatments.
Let’s dive into the key differences for piriformis syndrome vs. sciatica and what you can do to start feeling better.
Disclaimer: This content is for educational purposes and is not medical advice. Read the full disclaimer.
What is piriformis syndrome?
Let’s take a quick step back to understand how the piriformis muscle can irritate the sciatic nerve.
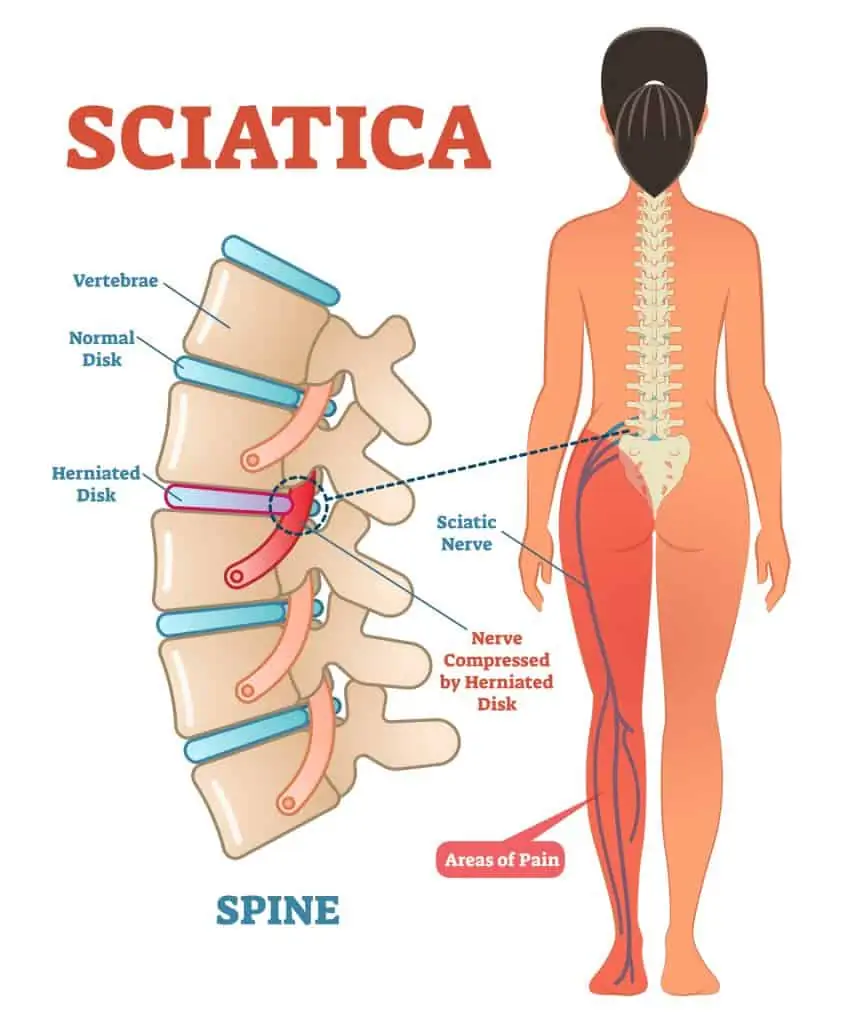
The sciatic nerve is the longest nerve in the body and originates from multiple nerve roots in the lumbar spine (lower back), forming the left and a right sciatic nerve.
Anatomy varies but the sciatic nerve generally exits around the piriformis muscle (at the back of the hip) and runs down the back of the thigh, splitting off into smaller nerves behind the knee. These branches then continue to the lower leg and foot.

The piriformis muscle runs from the sacrum to the back of the hip and helps to stabilize as well as externally rotate the hip.
Piriformis syndrome occurs when the sciatic nerve becomes irritated or compressed by the piriformis muscle.
There is some controversy about whether or not piriformis syndrome actually exists on its own, or if it’s part of a larger picture. It’s now also described as deep gluteal syndrome since there are many small muscles and structures in the area, and it’s difficult to drill down exactly which of these small structures is contributing to the issue.
Depending on who you ask, piriformis syndrome is either common or uncommon and is estimated to be the culprit in around 5% of sciatica cases.
Piriformis syndrome symptoms
Pain, numbness, or tingling can start in the back of the hip and radiate down the back of the leg. Lower back pain may also be present as the body attempts to compensate.
You may feel tenderness over the piriformis muscle, especially if you’ve tried to use a foam roller.
Typical piriformis syndrome symptoms can be felt with almost any motion requiring stabilization or movement of the hip, such as running, lunging, single-leg balance, stair climbing, or even sitting due to compression.
This area can also become irritated from sitting with crossed legs or items in the back pocket, such as a wallet.
Many structures in the back of the hip can be involved in sciatic nerve entrapment in the deep gluteal space.
Causes of piriformis syndrome (deep gluteal syndrome)
- Piriformis muscle spasm/spasm in other deep hip rotators
- Hip muscle weakness/imbalance
- Sacroiliac joint dysfunction
- Overtraining, especially on uneven surfaces
- Work that places you in an awkward or asymmetrical position for extended amounts of time
- Radiating pain from the lumbar spine/part of a more significant issue
- Trauma/bruising
- Previous hip injuries or surgeries
- Anatomical variations
Piriformis syndrome vs. sciatica
People are quick to call almost any pain down the back of the leg “sciatica” without further teasing out the details.
The confusing part is that piriformis syndrome can cause sciatica-like pain; however, not all sciatic symptoms are a result of piriformis syndrome.
The term sciatica is not a diagnosis but rather a description of a symptom (irritation of the sciatic nerve), and used by itself, is rather vague.
Many sciatica cases originate from the spine, such as with a disc bulge, causing inflammation of the lower spinal nerves (lumbar radiculopathy). This is sometimes referred to as a pinched nerve.
Common sciatica symptoms
- Moderate to severe pain in the lower back, back of the hip/buttock, and down the back of the affected leg
- Sensation changes such as numbness, tingling, pins, and needles, or prickly sensations
- Muscle weakness
- Pain and symptoms can be anywhere along the distribution of the sciatic nerve
As you can see, the symptoms of both are very similar with both causing leg pain, numbness, or tingling.
How can you tell them apart?
One of the significant differences found in an evaluation is how the pain is reproduced.
For example, piriformis syndrome is more likely to be reproduced with various tests moving the hip joint. In contrast, a true sciatica (e.g. from a disc herniation) will likely be aggravated by spinal movements and nerve tension tests.
It’s important to have an evaluation by a doctor and physical therapist for successful pain relief.
Causes of sciatica
- Lumbar herniated disc (slipped disc)
- Impingement at the lumbar nerve root
- Muscular spasm
- SI joint issues
- Piriformis syndrome
- Sciatic nerve compression
- Pregnancy
- Spinal stenosis
- Degenerative disc disease
- Spondylolisthesis
- Arthritis
- Limited hip mobility
- Trauma
- Malignancies or infections
Conditions such as vascular disease or peripheral neuropathy can mimic sciatic symptoms but are very different conditions.
Hamstring strains can also be mistaken for sciatic nerve pain, but a proper evaluation will tell them apart.
It’s also possible for multiple conditions to coexist, making diagnosis and treatment a little more challenging.
Don’t miss this article outlining plenty of tips on what to avoid when you have sciatica.
Conservative treatment
Sciatic nerve irritation can arise from several causes. Because the origins of these two conditions are different, treatment options for each will also look different.
Pigeon pose or figure 4 stretch are common stretches that are blindly recommended for sciatic pain. Unfortunately, it’s not as simple as recommending one stretch and calling it a day.
Many causes of sciatica originate in the lower spine. Therefore, simply stretching the hip may only bring some temporary relief without addressing the root cause of the pain.
It’s essential to be evaluated by your doctor and physical therapist to start on a program specific to your needs.
Conservative treatment may include:
- A comprehensive evaluation with possible imaging (X-ray, MRI, or CT scans)
- Specific strengthening and mobility/flexibility exercises (which will vary depending on the underlying causes)
- Activity modification and avoiding aggravating factors while rehabbing
- May include prescription or over the counter pain medication/anti-inflammatories
If you’ve never had physical therapy before learn what to know before you go here.
Is it sciatica or something else?
Several issues can cause or mimic sciatica pain, so it’s crucial to get evaluated to determine what to do next.
Don’t spend weeks trying to “stretch out” your piriformis with no improvement.
Tracking your symptoms and problem-solving with your providers can help get you on the right treatment plan to start seeing results.
REFERENCES
Davis D, Maini K, Vasudevan A. Sciatica. [Updated 2020 Nov 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507908/
Kean Chen C, Nizar AJ. Prevalence of piriformis syndrome in chronic low back pain patients. A clinical diagnosis with modified FAIR test. Pain Pract. 2013 Apr;13(4):276-81. doi: 10.1111/j.1533-2500.2012.00585.x. Epub 2012 Aug 2. PMID: 22863240.Hopayian K, Song F, Riera R, Sambandan S. The clinical features of the piriformis syndrome: a systematic review. Eur Spine J. 2010;19(12):2095-2109. doi:10.1007/s00586-010-1504-9
Martin HD, Reddy M, Gómez-Hoyos J. Deep gluteal syndrome. J Hip Preserv Surg. 2015 Jul;2(2):99-107. doi: 10.1093/jhps/hnv029. Epub 2015 Jun 6. PMID: 27011826; PMCID: PMC4718497.
Thiyagarajan, Senthilkumar. (2017). Pseudo Sciatica-It’s the Condition we really Treat Better than Medicine. Journal of Novel Physiotherapies. Volume 7. 10.4172/2165-7025.1000327.
Visser LH, Nijssen PG, Tijssen CC, van Middendorp JJ, Schieving J. Sciatica-like symptoms and the sacroiliac joint: clinical features and differential diagnosis. Eur Spine J. 2013;22(7):1657-1664. doi:10.1007/s00586-013-2660-5