This post may contain affiliate links. If you click through a link and make a purchase, I may receive a commission at no additional cost to you. As an Amazon Associate, I earn from qualifying purchases. Read the full disclosure here.
Does your Achilles frequently feel tight or painful?
That nagging feeling (especially after you were active) may be trying to tell you something (and the problem may not be just your Achilles).
Keep reading to discover some of the most common reasons why your Achilles always feels tight, what you can do about it, and why just resting or stretching isn’t the answer.
Disclaimer: This content is for educational purposes and is not medical advice. Read the full disclaimer.
Achilles tendon anatomy
Let’s start with a little anatomy refresh.
Fun fact: The Achilles tendon is the strongest tendon in the body and is designed to handle a lot of load, whether it’s walking, running, or jumping.
But tendons are more than thick connective tissue connecting muscle to bone. They store and release elastic energy throughout various phases of movement.
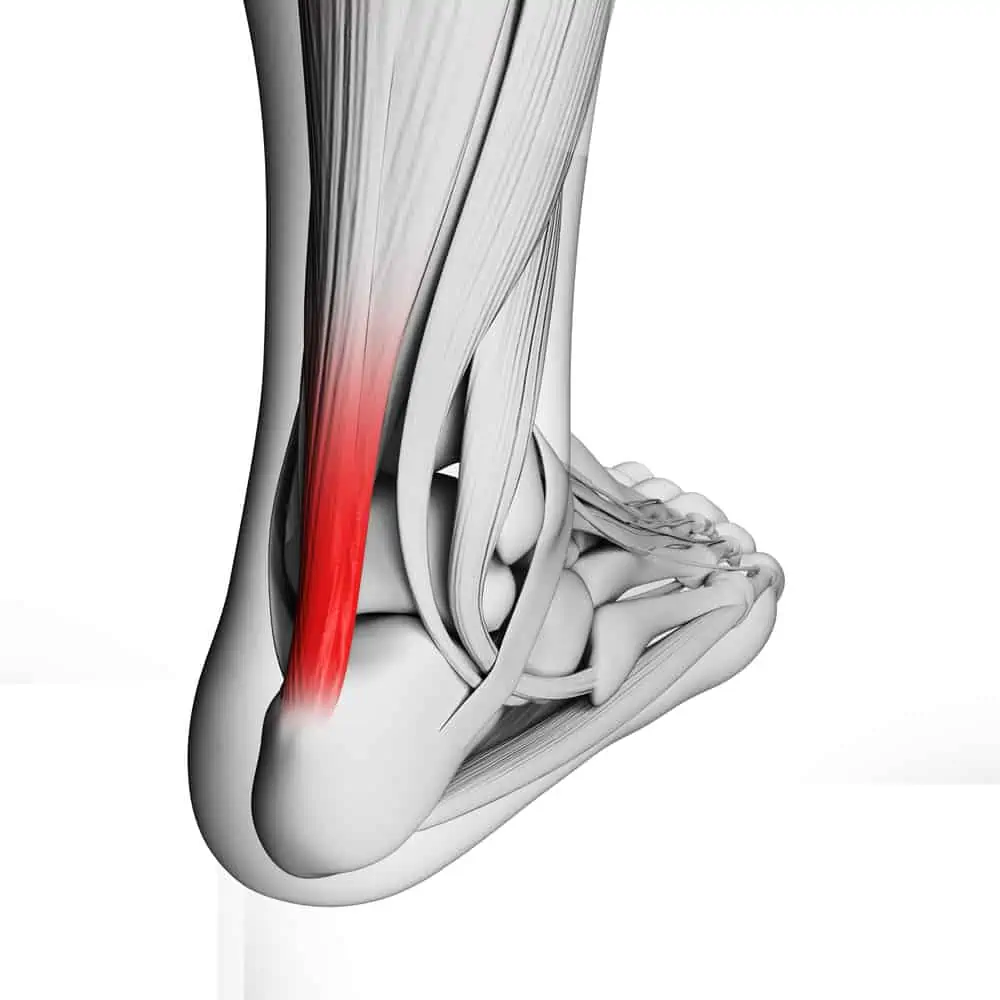
The Achilles tendon attaches the calf muscles to the heel. The gastrocnemius muscle is the larger and more visible calf muscle. It also crosses the knee joint, which is essential to note for optimal stretching and strengthening positions.
Beneath the gastroc is the soleus, also meaning “fish,” which is exactly what this muscle looks like. Together these muscles fuse into thick fascia that becomes the Achilles tendon.
The calf muscles function to plantarflex (point) the foot and rise up on your toes. The gastroc assists with running and jumping as well as pushing off when you’re walking.
These muscles also help with the first line of defense in keeping your balance during small postural sways.
What is Achilles tendonitis?
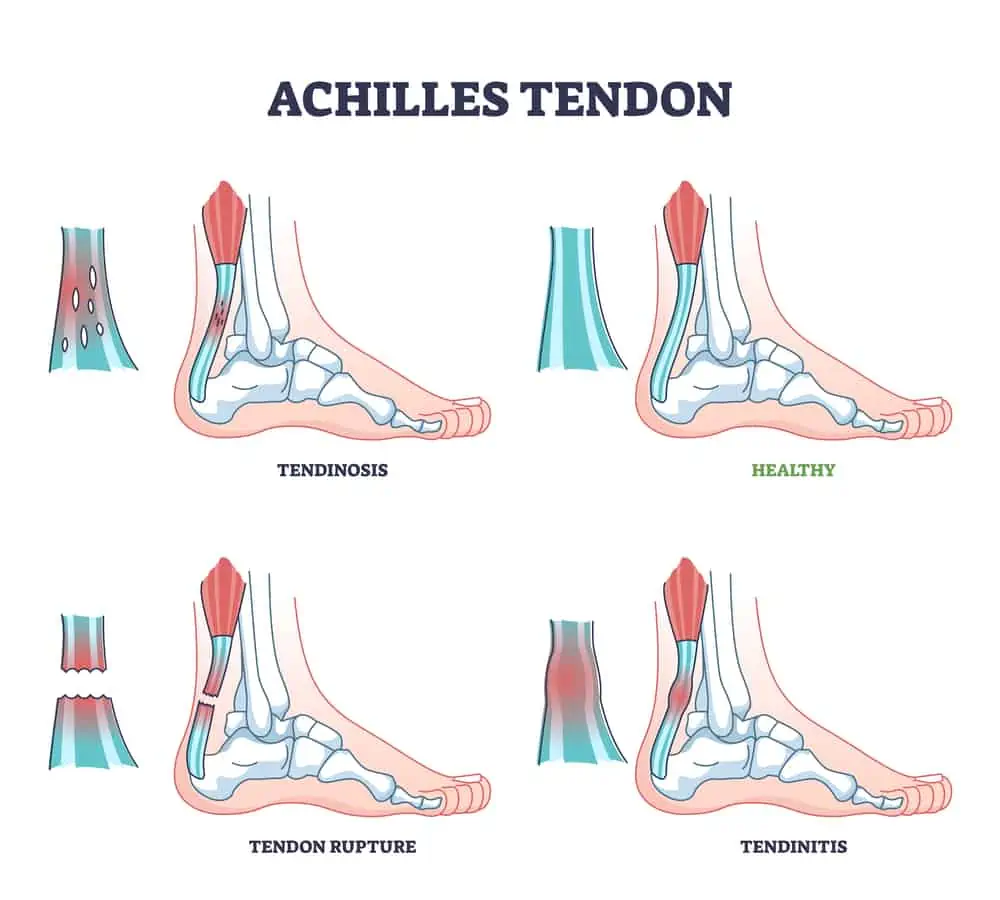
Achilles tendonitis (tendinitis, tendinosis, or tendinopathy) is overuse or irritation of the Achilles tendon. Tendonitis refers to more acute inflammation, and tendinopathy or tendinosis is more chronic in nature.
Either way, your Achilles hurts.
Symptoms of Achilles tendinopathy include pain and stiffness (especially in the morning, after sitting for long periods of time, or after exercise) at the point where the tendon inserts into the heel bone (insertional Achilles tendonitis) or further up the tendon.
Other noteworthy signs may be tenderness to touch or swelling, difficulty rising up on your toes, or pushing off during walking or running.
Achilles tendonitis tends to be more common in men, runners, or those who are ”weekend warriors” (as in being mostly sedentary during the week and saving all of your enthusiasm for the weekends).
There’s also an increased risk for Achilles tendon injury with certain antibiotics or corticosteroid use.
An Achilles tendon rupture is either a partial or full tear of the Achilles.
Why does my Achilles feel tight? (14 possible causes)
Injuries are often multifactorial, even though one instance often appears like the straw that broke the camel’s back. Unfortunately, we tend to demonize that one particular thing and swear it off forever, even though it may just have been the perfect storm of events.
Achilles injuries carry intrinsic and extrinsic factors, meaning things inside your body and outside factors like footwear, terrain, or training.
This gets tricky when pain comes on over time, including activities you’ve likely been doing for some time. So why does my Achilles feel tight “all of a sudden”?
When dealing with gradual onset pain, trial and error may be necessary to get to the root cause of the issue. Working with a doctor and physical therapist may help pinpoint the problems quicker.
As far as research goes, many of these risk factors have limited evidence individually, and “further research is needed,” what else is new?
Especially when it comes to overuse injuries, it can be pretty difficult to isolate exact causes definitively. The good news is that any healthcare provider should be taking into account the whole picture.
It’s also worth noting that not everything that falls out of “normal” doesn’t necessarily need to be fixed. (We see this all the time with professional athletes with variations in technique and function just fine.)
Sometimes “fixing” what’s not broken creates more extensive problems. Here are 14 potential contributors to why your Achilles always feels tight.
Related read: 5 Exercises To Avoid With Achilles Tendonitis
Calf muscle weakness
Injuries occur when the demand of a movement exceeds the current capacity of the particular tissue of the body.
As we’ve established before, the Achilles tendon gets a lot of work daily from everyday activities and exercise or sports. So ensure that your calf muscles are nice and strong to tolerate the demands of what you need.
Muscle weakness may also give you the perception of tightness, which is why only stretching misses a piece of the picture.
Strengthening is often cited as one of the best defenses against injuries, increasing the body’s ability to tolerate load. It provides valuable proprioceptive and neuromuscular input, increasing various tissues’ ability to adapt.
The video below demonstrates how to test calf muscle strength.
Ankle joint tightness
The ankle joint can also restrict movement into dorsiflexion (pulling your foot toward you.)
Decreased mobility in the talocrural joint (where the tibia, fibula, and talus form the ankle joint) will limit your step and stride length, your ability to squat deeply, and even limit your ability to descend stairs easily, step over step.
Ankle mobility is a good thing and is often overlooked as contributing to multiple lower body issues.
Check out this great video below for a quick, easy method to test your ankle mobility.
If your ankles and calves are feeling stiff, don’t miss my 20-minute yoga class focusing on flexibility for the foot and ankle. (And don’t forget to subscribe!)
Lack of extension at the big toe
This big toe needs a good 70 degrees of extension for us to transition through the gait cycle smoothly.
Extension at the big toe is a requirement for fluid walking and running and is often overlooked as a source of dysfunctional movement. If the range of motion is lacking, your body needs to engage other muscles and tissues earlier in the gait cycle, which can contribute to overuse.
There may also be an increased medial or lateral shift through the foot and ankle to compensate “around” a lacking area.
Check out the video below for some simple toe mobility exercises.
Keeping your feet strong and flexible can also help support the foot and ankle. Check out the related reads below.
Having a previous lower limb tendonitis or injury
There’s some evidence to suggest that having a previous lower limb injury (literally anywhere in the lower limb) such as tendonitis or a fracture can increase the risk for Achilles tendonitis.
When one injury hasn’t been addressed, hasn’t been fully rehabilitated, or left a residual deficit such as strength or mobility, there’s always the potential to develop overuse injuries elsewhere.
Related read: Surprising Reasons Why Your Plantar Fasciitis Isn’t Getting Better
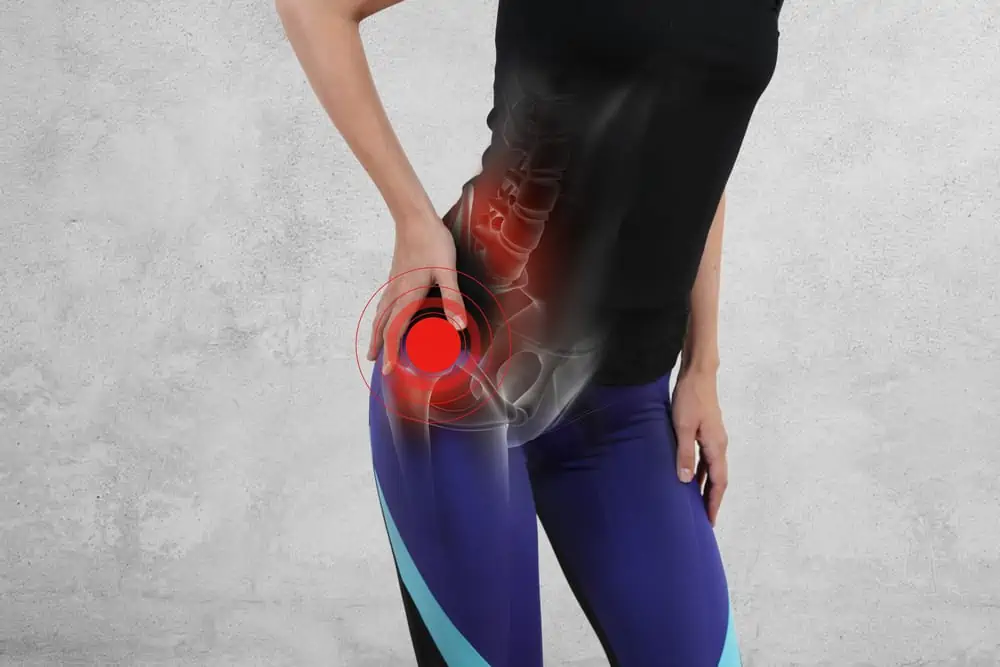
Limited hip mobility, especially into extension
Appropriate mobility at each joint is essential for good quality movement. A limitation in one area can affect gross movement patterns.
Hip mobility certainly gets attention in the fitness world for a good reason. Hip mobility in all directions is a significant contributor to how the rest of the kinetic chain will move.
Hip extension contributes to a comfortable step and stride length while walking and running. However, limited hip mobility may contribute to overuse injuries further down the chain.
Compensation for muscle weakness further up the kinetic chain
Doesn’t it seem like weak glutes are a culprit for many issues?
Well, that’s because, as the most powerful hip extensor muscle in the body, we can’t afford not to have the glutes pulling their weight.
Glute weakness may contribute to overuse injuries in many places, including the Achilles, hamstrings, and IT band.
Doing too much too soon (training errors)
Errors in training are one of the most common reasons for developing Achilles tendon issues.
Have you recently started increasing your running or decided to tackle more hills? A rapid change in training terrain or volume (hills, getting back to running, progressing too quickly) can jump-start overuse injuries.
Gabbett TJ suggests limiting weekly training increases to <10% to avoid increasing the risk for injuries. Give Garage Gym Review’s running pace calculator a try to help you progress safely.
Breakdown in mechanics, especially when fatigued
Are you good for a while, and then the pain sets in at some point? You might be experiencing a breakdown in mechanics when you’re fatigued.
If you’re a runner interested in seeing how your form changes when you’re fatigued, try recording yourself using the Hudl app.
You can record yourself running from multiple views, slow down the video, and inspect your form.
Recording yourself on the treadmill is an easy way to analyze your form. It may be helpful to record both when you’re fresh and fatigued; that way, you can compare your form.
If analyzing your gait sounds confusing, you can always see a physical therapist specializing in running injuries for a professional analysis and program.
You can also use your phone to record yourself performing other fitness movements to analyze your form.
Lack of adequate rest (training errors)
Injuries start to pile up if tissues are put on too much stress without adequate rest to repair and rebuild.
Take a look at your entire week, and be sure to spread out and vary your routines to avoid overloading tissues of the body.
Lack of a well-rounded treatment approach
Are you just sitting back in your comfy recliner waiting for your Achilles to feel better?
Unfortunately, only utilizing passive treatments doesn’t yield long-term results.
I’ll say it a little louder for the people in the back.
It’s not wrong to want to use an ice pack or sit back and stretch, but understand how this fits into an overall program to get you feeling better. The tricky part is that passive treatments may make you feel better temporarily, but it’s essential not to fall for this trap of thinking this is helping you in the long run.
RICE (rest, ice, compression, elevation) has been debunked for quite some time but still somehow circulating as a treatment for injuries. It’s not a bad start, but it doesn’t get you very far.
Another common mistake is that thinking “just stretching” will fix tendonitis.
If there’s anything that we’ve learned from recent research, it’s that tissues need to be progressively loaded to heal properly, especially tendons.
Exercises that promote flexibility, mobility, eccentric strengthening, and progressing loading of tissues have the best potential to get you better.
New advances in pain science indicate that pain isn’t a signal coming from a particular area; it’s an entire nervous system response. Strengthening introduces an element of neuromuscular control that’s necessary for proper healing and ultimately returning to a pain-free state.
Worn out, uncomfortable, or improper footwear
Do you have increased pronation or “flat feet”?
Flat feet can contribute to a host of foot and ankle problems, especially if accompanied by increased midfoot flexibility and intrinsic foot muscle weakness. This causes other structures to have to work extra hard to compensate.
Ensuring proper fitting footwear and arch support may help provide vital support to a less stable area.
Similarly, make sure you’re wearing the proper footwear for your activities. Uncomfortable or worn-out footwear may soon manifest as pain or tendonitis at the foot and ankle.
A shoe alone probably isn’t the only factor, but worn-out uncomfortable footwear isn’t helping the situation.
In addition, strengthening the feet may also help overcompensation in other areas.
Related read: Signs You’re Wearing The Wrong Shoes For Your Feet
Making adjustments to your form
Have you recently significantly changed your posture or alignment when you run or perform other fitness activities? This could be as simple as slightly changing the angle your toes are pointing.
It’s good to want to improve your form, but you also need to take into account individual anatomical variations.
We’re all a little asymmetrical, even from side to side. Sometimes, being “slightly off” is necessary for your body, and “fixing” something that isn’t broken may create more significant problems.
If you’ve tried to change your movement or form and developed other issues (more than just a minor temporary muscle soreness), it may not be the most optimal form for you.
Underlying medical issue or medication use
There’s some evidence linking specific medication and medical conditions to certain injuries, like Achilles tendinopathy.
Both the fluoroquinolones type of antibiotics and statins have been linked with Achilles tendon injuries.
Diabetes and psoriasis have also been documented as possible risk factors.
Do tight calves cause Achilles tendon issues?
Calf tightness is likely to come into the conversation about Achilles tendon issues.
Some studies don’t support tight calf muscles as a cause of Achilles tendonitis. It might not carry significant risk as a single factor, but it might have some merit as part of a total picture.
Did your tight calves contribute to developing Achilles tendonitis, or did the overload of the tendon contribute to tight calves?
The answer depends on who you ask, but I’m not sure anyone can say with a hundred percent certainty whether the chicken or the egg came first.
When we feel tightness in one area, we may start to compensate in our movement patterns. Then, before you know it, multiple locations feel tight.
We know that tightness in the calf muscles can restrict ROM of the ankle into dorsiflexion (pulling the foot toward you). In addition, issues with the Achilles tendon (that attaches to the calf muscles) can also restrict dorsiflexion.
Limited dorsiflexion can affect your stride length (how long of a step you can take) and flexibility with activities like going downstairs or even squatting. This can place additional strain on the Achilles tendon and plantar fascia.
So, I’ll just do a calf stretch, right?
Hold on a minute; too much passive stretching can tug at the Achilles insertion. Constant stretching may worsen the issue if this area is already irritated, including a delayed pain response to stretching.
Not to mention, Achilles tendonitis may give you the perception of your calves feeling tight, even if they aren’t.
Flexibility is part of recovering from Achilles pain, but it isn’t the only part. Flexibility is relatively passive, and passive treatments alone don’t yield long-term results.
Exercises that promote flexibility, mobility, eccentric strengthening, and progressing loading of tissues have the best potential to get you better.
So what if your calves still feel tight? You can also try using a foam roller, massage ball, muscle scraping, or mobility exercises.
A massage gun also works well for tackling those tight muscles. Read about my favorite massage gun Hydragun, here.
Check out these other in-depth articles covering these topics:
- What is muscle scraping?
- How Does Foam Rolling work?
- How to Stretch Tight Calves
- Vibrating Foam Rollers vs. Massage Guns
When to see a doctor
Here are some reasons why you might want to see an orthopedist or even a foot/ankle specialist for your Achilles pain.
- New or sudden onset pain, swelling, or weakness
- Inability to rise on your toes or push off while walking
- You feel a divot or lump in the tendon
- You’ve tried all the conservative treatments, and nothing seems to be working
You can also try physical therapy if there are no immediate red flags (such as a sudden loss in plantar flexion strength). A physical therapist can evaluate you for not-so-obvious underlying causes of your pain.
Many states now have direct access to physical therapy, allowing you to go directly to a physical therapist without a prescription.
You may need to follow up with your doctor within 30 days (varies by state) to continue PT, but this allows you to access rehab services faster.
It may also depend on the particulars of your insurance plan. Call your local PT office for information specific to your area.
If you’ve never had physical therapy before, don’t miss this article outlining how to prepare for your first appointment and where you can get a free checklist!
Wrapping up
Achilles tendon pain or stiffness can limit your ability to be active.
As with most cases of tendonitis, just stretching or sitting around waiting for things to improve isn’t the best approach.
Ignoring an injury long-term could lead to further tendon damage.
Be sure to get a comprehensive evaluation of your Achilles injury to tackle all possible contributing factors to get better fast.
References
Baik S, Lau J, Huser V, et alAssociation between tendon ruptures and use of fluoroquinolone, and other oral antibiotics: a 10-year retrospective study of 1 million US senior Medicare beneficiariesBMJ Open 2020;10:e034844. doi: 10.1136/bmjopen-2019-034844
Egger AC, Berkowitz MJ. Achilles tendon injuries. Curr Rev Musculoskelet Med. 2017 Mar;10(1):72-80. doi: 10.1007/s12178-017-9386-7. PMID: 28194638; PMCID: PMC5344857.
Gabbett TJThe training-injury prevention paradox: should athletes be training smarter and harder?British Journal of Sports Medicine 2016;50:273-280.
Kim GK. The Risk of Fluoroquinolone-induced Tendinopathy and Tendon Rupture: What Does The Clinician Need To Know? J Clin Aesthet Dermatol. 2010 Apr;3(4):49-54. PMID: 20725547; PMCID: PMC2921747.
Medina Pabón MA, Naqvi U. Achilles Tendonitis. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538149/
O’Neill S, Watson PJ, Barry S. A DELPHI STUDY OF RISK FACTORS FOR ACHILLES TENDINOPATHY- OPINIONS OF WORLD TENDON EXPERTS. Int J Sports Phys Ther. 2016 Oct;11(5):684-697. PMID: 27757281; PMCID: PMC5046962.
van der Vlist AC, Breda SJ, Oei EHG, et alClinical risk factors for Achilles tendinopathy: a systematic reviewBritish Journal of Sports Medicine 2019;53:1352-1361.
Witvrouw E, Mahieu N, Roosen P, McNair P. The role of stretching in tendon injuries. Br J Sports Med. 2007 Apr;41(4):224-6. doi: 10.1136/bjsm.2006.034165. Epub 2007 Jan 29. PMID: 17261561; PMCID: PMC2658965.