This post may contain affiliate links. If you click through a link and make a purchase, I may receive a commission at no additional cost to you. As an Amazon Associate, I earn from qualifying purchases. Read the full disclosure here.
Tired of plantar fasciitis feeling like a knife driving through your foot with every step? Then this article is for you.
Plantar fasciitis affects approximately 2 million people per year and has long been known as a painful and tricky injury to treat. Whenever I see a patient for plantar fasciitis, I need to provide a lot of education to un-do the misconceptions that Dr. Google has circulating.
There’s a laundry list of first-line treatment tactics, but what happens when plantar fasciitis won’t go away? Don’t resolve yourself to forever pain or invasive procedures just yet! To stop this annoying heel pain in its tracks, you need to look beyond the foot.
Today you’ll learn the not-so-obvious causes of plantar fasciitis for a comprehensive approach to beat the pain and get back to life!
- What is plantar fasciitis?
- Plantar fasciitis symptoms
- What causes plantar fasciitis?
- Common plantar fasciitis treatments
- The surprising reason why your plantar fasciitis won’t go away
- Not-so-obvious causes of plantar fasciitis
- What’s the best exercise for plantar fasciitis?
- Can toe spreaders help plantar fasciitis?
- Orthotics for plantar fasciitis
- FAQ about plantar fasciitis
- Plantar fasciitis prevention tips
- Will my plantar fasciitis ever go away?
Disclaimer: This content is for educational purposes and is not medical advice. Read the full disclaimer.
What is plantar fasciitis?
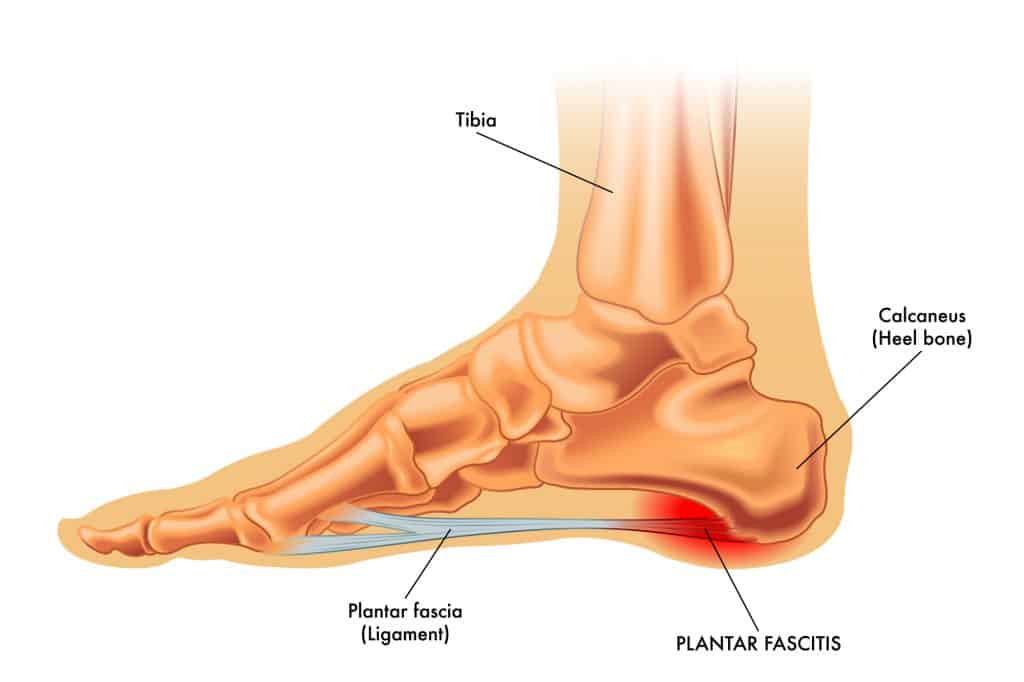
The plantar fascia is a thick band of connective tissue that runs along the arch of the foot to the heel bone. It functions to support the arch and transfer force through the foot and lower leg during movement.
When the plantar fascia ligament is asked to pull more than its fair share, it’ll let you know, in the form of stabbing pain with every step.
Plantar fasciitis is an inflammation of the fascia at its insertion point on the heel. If the pain becomes chronic, for example, months to years, the condition may be called plantar fasciosis.
There’s also some newer evidence that chronic plantar fasciitis is related to decreased blood flow, which affects the body’s ability to get fresh blood carrying oxygen and other reparative cells to the area to initiate tissue healing.
This finding argues that chronic cases are less about inflammation and more about tissue degeneration, making the condition more multifactorial than originally thought.
Plantar fasciitis symptoms
A hallmark sign of plantar fasciitis is heel pain/arch pain first thing in the morning. The pain may improve as the tissues warm up and may worsen with prolonged walking/standing.
During normal activities, the tissues are warm and move through their full range of motion (ROM).
After sleeping for several hours with your feet in a more relaxed position, those first few steps may cause severe pain as the inflamed tissues attempt to warm up and move through their full range of motion again.
Plantar fascia pain can also feel worse after prolonged standing and walking activities.
What causes plantar fasciitis?
Though it may seem like plantar fasciitis creeps up overnight, several background issues can contribute over time, sometimes for weeks or months.
- Anatomy/structure of the foot
- Poor footwear choices
- Altered movement mechanics (due to other injuries, tightness, or weakness) that change the way we walk
- Other lower limb injuries/tendinopathies
- Ramping up fitness activities too quickly, especially running
- Spending a lot of time standing/walking
- Wearing high heels
- Obesity
Related read: 11 Signs You’re Not Wearing the Best Shoes for Your Feet
What’s the difference between plantar fasciitis and heel spurs?
These two often become confused. It’s a common misconception that heel spurs cause plantar fasciitis; the truth is, it’s likely to be the other way around.
A heel spur (sometimes called a bone spur) is a bone or calcium deposit that grows in the heel (calcaneus) where the plantar fascia inserts, in response to repetitive stress. Heel spurs can develop in response to chronic plantar fasciitis, but the heel spur itself doesn’t often cause pain.
How long does it take for plantar fasciitis to heal?
Unfortunately, plantar fasciitis improvement is often slow, especially if you ignore the pain for a few months and allow the condition to become chronic.
With the right treatment, plantar fasciitis can heal in 6-12 months.
However, The earlier you address symptoms, the faster you can see results.
Common plantar fasciitis treatments
Here are some common first-line treatments often used to decrease plantar fasciitis pain.
- Rest/activity modification
- Massage – rolling the arch on a trigger point ball
- Calf stretching
- Scraping therapy
- Orthotics or over-the-counter shoe inserts
- Heel cups
- Arch sleeve or arch wraps
- Taping
- Ice packs
- Anti-inflammatory medication
- Night splint
These treatments can be a helpful starting point and offer some short-term pain relief, but if you find yourself asking why won’t my plantar fasciitis go away, there may be more to the puzzle.
Related read: How To Apply Kinesiology Tape So It Actually Stays On & Scraping Therapy For Plantar Fasciitis – Does It Speed Up Recovery?

The surprising reason why your plantar fasciitis won’t go away
Chronic heel pain can be very frustrating. It’s easy to think, I have foot pain, so I’ll treat my foot.
It seems logical, right? Except, it’s not.
Successful treatment for plantar fasciitis pain is often a multi-pronged approach.
Yes, it’s important to decrease inflammation locally and improve foot/ankle range of motion. That’s where many of those first-line treatments come in handy.
But it turns out; the foot is connected to the rest of your body. When plantar fasciitis won’t disappear, it’s time to look elsewhere.
Many other factors further up the kinetic chain can manifest as plantar fasciitis. If you don’t look beyond the foot, you’ll never find other contributors to the issue, perpetuating the chronic pain cycle.
Treat the actual problems instead of just the symptoms.
All the ice and foot massages in the world won’t fix the issue if there are other contributors, for example, the hip. It’s a delicate dance of decreasing local inflammation while restoring healthy movement.
The best way to get rid of plantar fasciitis is to also look beyond the foot.
Related read: What Not To Do With Plantar Fasciitis
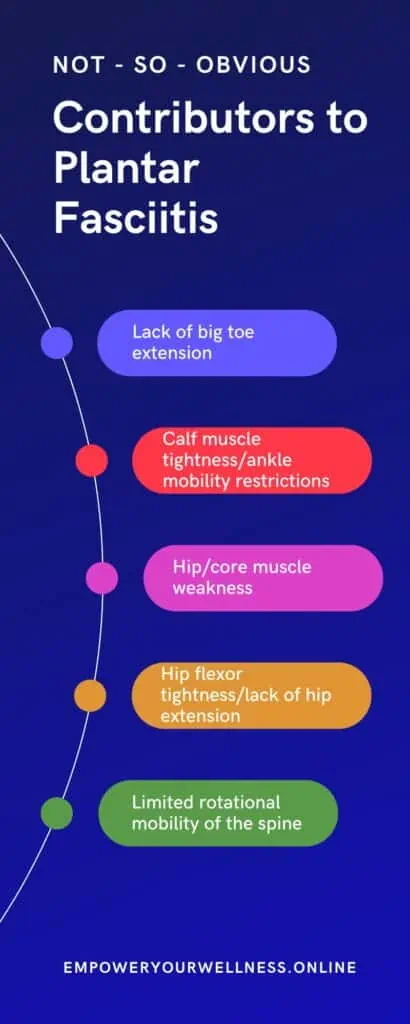
Not-so-obvious causes of plantar fasciitis
Any area of the body can change how we move and walk. When movements are altered in a dysfunctional way, it can lead to overuse issues.
Here are some examples of how other structures can cause plantar fasciitis that won’t go away. Evaluating these areas can provide a key puzzle piece in plantar fasciitis relief.
Lack of extension at the big toe
I know, I just said you need to look outside of the foot. We’ll get there.
Extension at the big toe is a requirement for fluid walking and running and is often overlooked as a source of dysfunctional movement. If the range of motion is lacking, your body needs to engage other muscles and tissues earlier in the gait cycle, which can contribute to overuse.
Lack of extension range of motion here can contribute to a host of overuse injuries at the foot/ankle and beyond.
Intrinsic foot muscle weakness
The feet have plenty of super small muscles to help with maintaining the arch of the foot and, in general keep our feet doing their job of getting us around all day.
Poor footwear choices and a lack of focus on foot strength can lead to intrinsic muscle weakness, which, in turn, can lead to overuse and pain.
For some, strengthening the small muscles of the feet PLUS focusing on the hips can go a long way in keeping plantar fasciitis pain away for good.
Calf muscle tightness / ankle mobility issues
Calf muscle tightness or the perception of a tight Achilles tendon is a common contributor to plantar fasciitis.
Tightness in the calf muscles (gastrocnemius and soleus) can restrict ROM of the ankle into dorsiflexion (pulling the foot toward you). Issues with the Achilles tendon (that attaches to the calf muscles) can also restrict dorsiflexion.
Ankle mobility restrictions can also contribute to calf muscle tightness. Limited dorsiflexion (pulling your foot toward you) can affect your stride length (how long of a step you can take) and flexibility with activities like going downstairs or even squatting. This can place additional strain on the plantar fascia and decrease the fluidity of your gait (walking) pattern.
To learn different methods to stretch the calf muscles, check out the ankle/foot flexibility library and How To Stretch Tight Calves.
You can also try my 20-minute ankle flexibility flow below for exercises aimed at tight ankles and calves.
Best tools for tight calf muscles
Here are a few of my favorite tools to tackle tight calves.
Here’s an awesome adjustable calf stretch incline board. This tool is an easy way to get a great stretch and allows you to change the angle as your flexibility improves – a crowd favorite in physical therapy clinics. Even the physical therapists would stand on it several times daily because it feels so good.
What I love about an adjustable incline board is the option to increase the range of motion as you become more flexible.
Muscle scraping is also a great way to address problem areas at home.
Muscle scraping tools offer a different type of soft tissue mobilization that can’t be accomplished by hand. My Sidekick tools were tremendously helpful during the pandemic when getting a massage was not an option.
Muscle scraping tools are used for soft tissue such as muscle and fascia to break up scar tissue and improve soft tissue mobility. These tools come in a variety of shapes to contour various body parts. And, they feel amazing!
Scraping is an excellent adjunct to your regular foam rolling routine, along with stretching and mobility exercises for best results. Using a scraping tool for the calves and feet can help with soft tissue mobility and provide some relief.
The brand that I use is Sidekick. The Eclipse tool is perfectly shaped for calves and feet. The Swerve also works for these areas, in addition to being a great all-around tool.
Click here to read my full review of Sidekick plus learn more about muscle scraping. You can also check out this article specifically about scraping therapy and plantar fasciitis – does it speed up recovery?

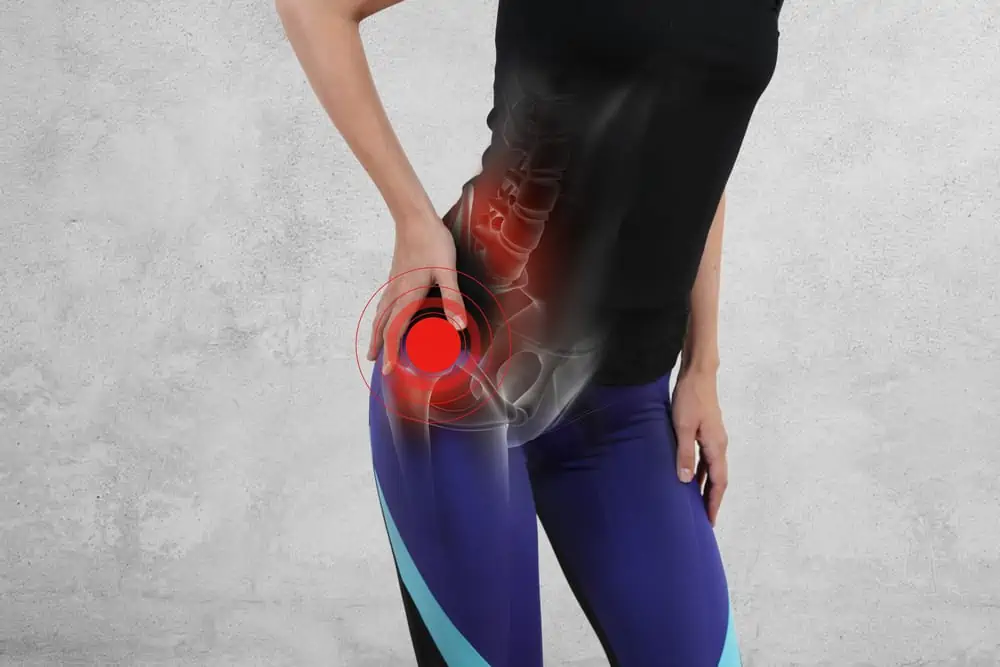
Hip/core muscle weakness
It seems like core strengthening is some magical fix for everything, doesn’t it? Let me explain.
The glute max is the most powerful hip extender in the body, and also a common muscle group to find weakness, especially with prolonged sitting.
Glute max helps propel you forward while walking. Weakness in the glutes can contribute to a host of issues, including plantar fasciitis.
But the hip is so far away from the foot!
Sounds crazy, right?
It’s not that far-fetched from a movement perspective. Remember, it’s all connected. Strengthening the glutes can contribute to plantar fasciitis relief.
The body will keep moving down the line (or up the line), looking for other tissues to pick up the slack. After a while, these tissues become overworked and inflamed.
These loop resistance bands are an awesome way to build hip and glute strength – lateral walks and clamshells are two of my favorite exercises!
Glute bands are also heavy-duty fabric resistance bands designed to work these strong muscles without heavy equipment.

Hip flexor tightness
The hip flexors function to propel your leg forward while walking and to bring the knee toward your chest. Psoas, the major hip flexor, also plays a role in core stability.
Tightness and weakness are usual suspects in those with sedentary jobs, spending extended hours sitting.
Lack of full ROM of the hip flexors can limit how far your hip extends (the opposite direction of flexion). Hip extension is essential for walking. If it’s limited, that can create extra work for the calf and foot.
Spoiler alert, it may even be on the opposite side of the body!
For ideas on how to stretch the hip flexors, check out the hip flexibility library.
Related Read: How Do You Fix Tight Hip Flexors?
Limited rotational mobility of the spine
Have you ever wondered why we swing our arms when we walk? That reciprocal movement helps us walk easier and with more fluidity.
Now try taking a few steps holding your arms at your sides, keeping your upper body still.
Awkward right?
You may have noticed you didn’t move as fluidly, and you had to work a little harder to get going, which was more work for the feet and ankles.
Check out the spine flexibility library.
What’s the best exercise for plantar fasciitis?
It depends on what’s causing your plantar fasciitis.
It may be beneficial to team up with a podiatrist and physical therapist simultaneously for the best results.
If the condition is chronic, it’s likely there is more than one issue at play.
Unless you have another injury that you can trace back to, it can be challenging to figure out the underlying cause.
Which came first, the chicken or the egg?
The world may never know, but if you don’t address all the causes, you’ll spend years rolling your foot on a tennis ball, wondering why the pain never goes away.
It’s essential to get evaluated by a physical therapist that will assess your movement as a whole to call out these underlying offenders and design a comprehensive program.
The longer an injury lingers, the more difficult it becomes to resolve. Inflammation becomes chronic, tissue damage occurs, and bad movement patterns breed more bad patterns, leading your body to feel this is the new normal.
It’s worth it to exhaust all the conservative treatment options before jumping into surgery.
Read What is Physical Therapy & How Can It Help You and grab the free PT checklist in the box below!
Can toe spreaders help plantar fasciitis?
Shoes that cramp your toes together not only affect the mechanics of your feet but can also compress nerves and blood vessels.
With new evidence that restricted blood flow may be one of the culprits in chronic cases, trying some toe spreaders may have some benefit.
These soft gel toe separators by Mind Bodhi are super comfortable and can help improve mobility and strength for stiff and weak feet.
You can read the full article on toe spreaders for plantar fasciitis here.
Orthotics for plantar fasciitis
Custom orthotics and over-the-counter insoles can be a great option along the plantar fasciitis journey.
An orthotic supports the foot’s arch, which also positively affects the alignment of other joints of the body from the ground up.
If you have particular needs, you will need to see a podiatrist for custom orthotics. The downside is they can be costly (in the neighborhood of $400-$600 per pair). Insurance limits how many pairs you can have, if they cover them at all.
Related read: Are Birkenstocks Good For Plantar Fasciitis?
Best over-the-counter orthotics for plantar fasciitis
For over-the-counter affordable, high-quality insoles, I recommend Superfeet.
They offer different types of insoles for all activities and are cost-effective enough to have several pairs to go around in your shoe collection.
An over-the-counter heel cup may also provide some much-needed plantar fasciitis relief. A silicone heel pad can provide extra cushioning and support to cradle a painful heel and decrease pain.
Superfeet insoles are available on Amazon, but they sometimes run sales on their website.
New Superfeet customers can get 10% off with email sign-up – click here and use code WELCOME10.
FAQ about plantar fasciitis
In this section, I answer some of the most commonly Googled questions about plantar fasciitis.
Does stretching make plantar fasciitis worse?
Stretching, especially for the calf muscles can help with plantar fasciitis.
The plantar fascia itself isn’t a muscle, it’s a thick band of tissue that helps support the arch of the foot and facilitate proper foot mechanics with walking.
Aggressive stretching or massage of the plantar fascia may make symptoms feel worse.
Does walking make plantar fasciitis worse?
Too much walking, especially when coupled with poor footwear choices, can make plantar fasciitis worse.
Activity modification and supportive footwear are key pieces of healing your plantar fasciitis.
Why is plantar fasciitis worse in the morning?
A hallmark sign of plantar fasciitis is pain that’s worse in the morning with the first few steps and may gradually improve with movement.
During the night, our feet are in a more relaxed position, which keeps the plantar fascia in a shortened position. We’re also not moving around so there isn’t as much blood flow and circulation, so tissues aren’t warmed up.
Those first few steps stretch the plantar fascia again, and this can be painful for irritated tissue.
Should I stay off my feet with plantar fasciitis?
It’s natural to want to stay off of a painful foot. However, as with most injuries, rest alone usually does more harm than good.
Resting won’t fix other biomechanical issues contributing to your pain (such as tightness, weakness, or poor movement patterns) and will likely prolong your injury.
Get evaluated by your doctor and physical therapist to learn the right amount of activity modification and a proper treatment plan so that you can start making progress.
What happens if you ignore plantar fasciitis?
If plantar fasciitis is left untreated, the condition can turn chronic and remain painful. If you ignore plantar fasciitis, your pain will likely get “louder” and less easy to ignore.
As you begin to compensate for painful feet, your mobility can change and cause other injuries further up the kinetic chain, such as knee pain, hip pain, or even lower back pain.
Chronically inflamed plantar fascia can also tear or rupture, possibly requiring surgery.
It’s never a good idea to ignore pain. This can lead to further tissue damage and greater difficulty and complexity in resolving your symptoms.
Why does it take so long for plantar fasciitis to heal?
Plantar fasciitis has a reputation for being difficult to treat. The longer a condition is present, the longer it takes to heal.
It can be difficult to find a good balance of activity modification and treatment when you have other life obligations.
Getting symptoms addressed early and taking a multidisciplinary treatment approach can help you see results faster.
Is plantar fasciitis a form of arthritis?
Plantar fasciitis is not the same as arthritis.
Plantar fasciitis is an inflammation of the plantar fascia tissue. Arthritis is the swelling or tenderness of a joint.
Plantar fasciitis and arthritis may exist alongside each other, but the diagnoses involve different types of tissues in the body.
What helps plantar fasciitis heal faster?
Getting a proper diagnosis and starting treatment early will help plantar fasciitis to heal faster.
Ignoring symptoms to the point where they become chronic and focusing on poor-quality treatments that chase symptoms and ignore the root cause of the pain can delay healing.
Is soaking feet in hot water good for plantar fasciitis?
Soaking your feet in hot water may temporarily relieve pain and soreness, however, passive modalities like heat and cold only yield temporary relief and do not address the root cause of pain.
It’s not bad to use this treatment in conjunction with other treatments, however, it’s essential to understand that soaking your feet alone will not cure plantar fasciitis.
Can I wear sandals if I have plantar fasciitis?
Flat flip-flops are usually discouraged with plantar fasciitis due to the lack of arch support and extra gripping that your toes need to do to keep the sandal from flying off of your foot.
That being said, no one likes being stuck in sneakers in the summertime or during a beach vacation. If you’re suffering from plantar fasciitis pain, I recommend checking out a supportive sandal like Birkenstock or Fitflop to keep your feet happy in the warmer months.
Get 20% off of your Fitflop order here.
Plantar fasciitis prevention tips
Here are some easy steps you can take to decrease your chances of developing plantar fasciitis.
- Wear shoes with good support and shock absorption; replace them at regular intervals
- Add orthotics or over the counter insoles
- Maintain a good balance of flexibility and strength for healthy movement
- Don’t ramp up training too quickly, for example, significant increases in running mileage
- Maintain a healthy weight
- Don’t let injuries linger, seek care sooner than later
Will my plantar fasciitis ever go away?
Plantar fasciitis can be a very painful condition and chronic foot pain can hold you back from enjoying your life.
Human movement is extraordinarily complex and poor movement patterns further up the kinetic chain can manifest as plantar fasciitis.
The best plantar fasciitis treatment is a multi-disciplinary approach and some trial and error.
Other than ignoring the pain, the worst thing you can do is the same failed treatment repeatedly and wonder why you’re not getting results.
It’s worth exploring all conservative (non-surgical) options before jumping into more invasive treatments.
Remember to look outside of the foot to ditch painful plantar fasciitis!
You might also like:
- 11 Signs You’re Wearing the Wrong Sneakers
- How to Choose the Right Sneakers for Your Workout
- Mobility vs Stability vs Flexibility – How to Unlock Healthy Movement
- You Can’t Stretch the IT Band (& What To Do Instead)
References
Bolgla LA, Malone TR. Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice. J Athl Train. 2004;39(1):77-82.
Jacobs, J.L., Ridge, S.T., Bruening, D.A. et al. Passive hallux adduction decreases lateral plantar artery blood flow: a preliminary study of the potential influence of narrow toe box shoes. J Foot Ankle Res 12, 50 (2019). https://doi.org/10.1186/s13047-019-0361-y
Lewis RD, Wright P, McCarthy LH. Orthotics Compared to Conventional Therapy and Other Non-Surgical Treatments for Plantar Fasciitis. J Okla State Med Assoc. 2015;108(12):596-598.
Miller LE, Latt DL. Chronic Plantar Fasciitis is Mediated by Local Hemodynamics: Implications for Emerging Therapies. N Am J Med Sci. 2015;7(1):1-5. doi:10.4103/1947-2714.150080
Rathleff MS, Mølgaard CM, Fredberg U, et al. High-load strength training improves outcome in patients with plantar fasciitis: a randomized controlled trial with 12-month follow-up. Scand J Med Sci Sports. 2015;25(3):e292–e300.
Santos BD, Corrêa LA, Teixeira Santos L, Filho NA, Lemos T, Nogueira LA. Combination of Hip Strengthening and Manipulative Therapy for the Treatment of Plantar Fasciitis: A Case Report. J Chiropr Med. 2016;15(4):310-313. doi:10.1016/j.jcm.2016.08.001
Scherger JE, Spinoso A, Carlson W. Use of muscle strengthening to treat plantar fasciitis. ACSM Health Fitness J. 2017;21(2):37–38.




My plantar fasciitis is very painful. Thanks for the tips.
Love this! Thanks for sharing this valuable info ?
Thanks for reading!