This post may contain affiliate links. If you click through a link and make a purchase, I may receive a commission at no additional cost to you. As an Amazon Associate, I earn from qualifying purchases. Read the full disclosure here.
A lumbar herniated disc can be a painfully scary experience.
It’s incredibly frustrating to figure out how to get on with your daily life when something so simple as bending over to tie your shoes can leave you in excruciating pain.
But what activities should you avoid with a herniated disc?
In this article, I’ll explain all the details behind disc herniations (and what to avoid) so you get better faster.
Disclaimer: This content is for educational purposes and is not medical advice. Read the full disclaimer.
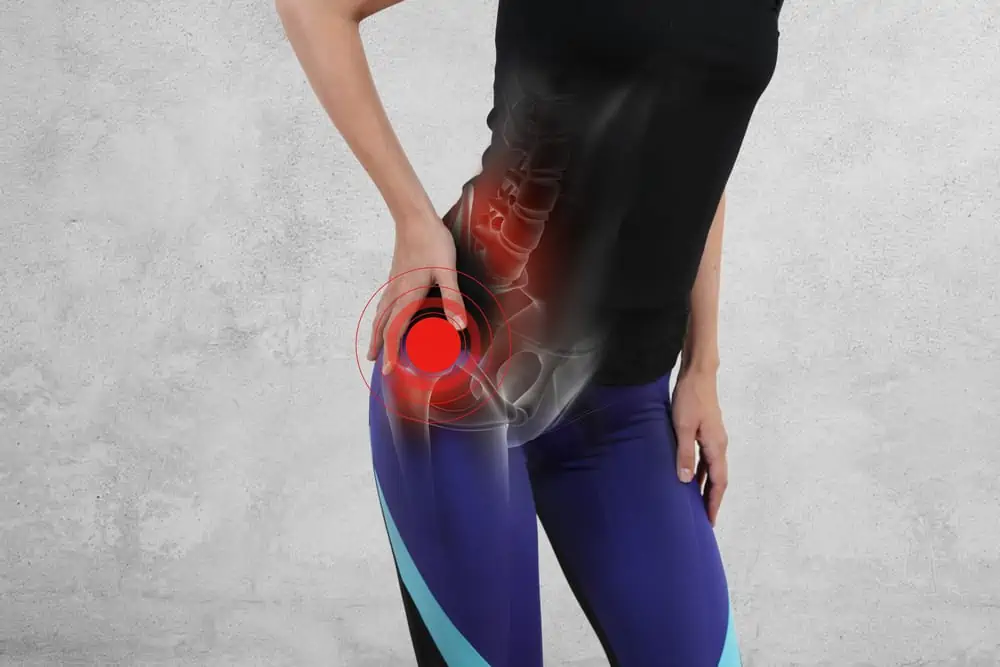
What is a herniated disc?
Let’s first take a tour of the lumbar spine to unpack the mystery behind herniated disc pain.
Why does it hurt so much in one position but not another? Getting some insight into the mechanics will help you move better with less pain.
The lumbar spine has five vertebrae and connects the thoracic spine to the sacrum.
Lumbar spine vertebrae are large and stable to absorb shock at this vital crossroad between the hips and core, yet still allow for movement.

Small muscles and thick ligaments wrap this area securely to tolerate exercise and everyday activities.
Between each vertebral body is an intervertebral disc. Discs help to cushion movements and absorb shock.
Each disc has a fibrous outer layer (annulus fibrosus) and a gel-like nucleus (nucleus pulposus). A jelly donut is a good visual, although many don’t like this comparison.
Comparing an intervertebral disc to a delicate fluffy doughnut doesn’t reflect how tough and rugged the outer layer actually is.
This comparison makes you think that the spine is fragile, and one wrong move will result in leaking jelly all over the place (and you can bet it won’t be delicious strawberry).
As the spine moves, the nucleus pressure shifts to keep the forces balanced.
For example, with extending (backward bending), the nucleus shifts forward as the vertebral bodies open, and with flexion, the nucleus moves back as the spine compresses. Injuries and degenerative changes can alter these pressure shifts.
Because we do many activities that require flexion or forward bending (even posture while sitting), it’s common for discs to herniate toward the back.
Herniated disc vs. bulging disc
There are a lot of terms thrown around when it comes to the spine, including some colloquial phrases that are rather silly like “slipped disc” or “my back went out.” Technically, discs don’t “slip” and your back is still there.
But what’s the difference between a bulging disc and a herniated disc?
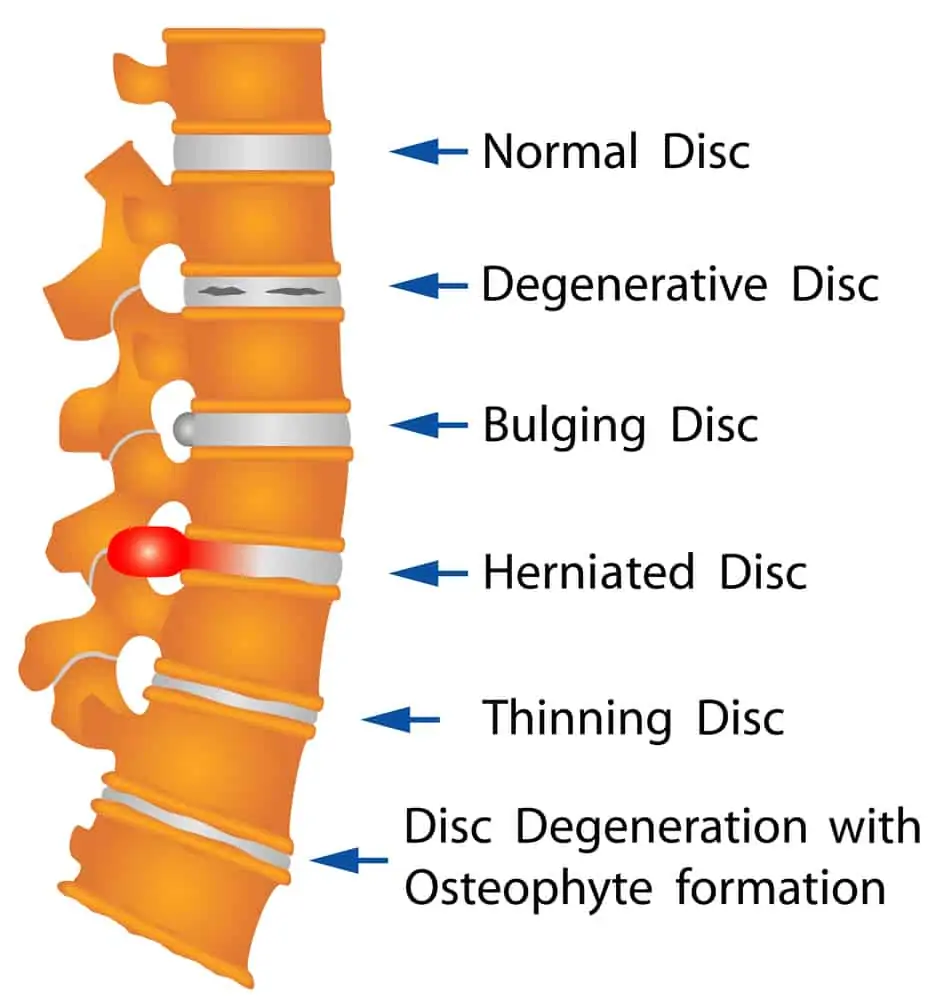
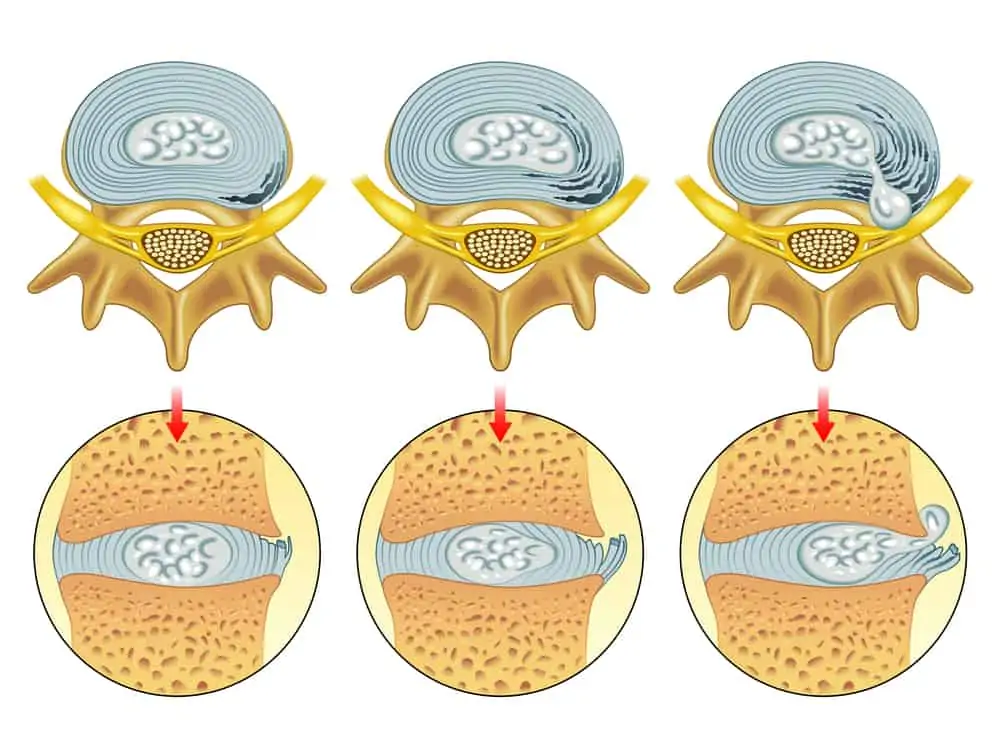
A bulging disc is just a slight protrusion (or bulge) of the disc’s fibrous outer layer.
A disc bulge may not have symptoms and is common with normal age-related changes as discs lose fluid, and the outer cartilage layer becomes less pliable.
With a herniated disc (also called a “slipped disc” or ruptured disc), the outer layer becomes cracked, and the nucleus pushes its way out.
It’s most common to see disc herniations in the cervical spine (neck) and lower lumbar spine (low back). 95% of all lumbar herniated discs are between L4-L5 or L5-S1. (Dydyk AM et al.)
A disc herniation can happen with one acute injury or as a result of degenerative changes and is more likely than a disc bulge to cause pain.
As you can imagine, there isn’t much space to work with, so a herniation can easily compress spinal nerves (often called a pinched nerve) and cause back pain, radiating pain, numbness/tingling, or muscle weakness.
A lumbar herniated disc can cause the symptom “sciatica,” but not all things casually called sciatica are due to a herniated disc.
You can read more about this critical distinction and what to avoid with sciatica in this article.
It’s also important to note that bulges and even small herniations don’t always equal pain. An MRI might pick up on something that you’re not even having symptoms of, leading to fear and movement avoidance.
Similarly, imaging may not show much at all, which is even more frustrating when you’re looking for answers.
Can herniated discs heal on their own?
Yes, in most cases.
According to a 2016 study published in the British Medical Journal, 90% of sciatica cases due to lumbar disc herniation resolve with conservative measures. Conservative treatment also carries a lower risk of complications than surgery and is often preferred by patients.
The study also notes that pain was relieved more quickly in patients who had surgery, but there was no difference between surgical and non-surgical patients at the three-month mark.
The right course of treatment for you will be between you and your doctor.
*If you notice a sudden or severe loss of strength in any area, significant bowel/bladder changes, or numbness in the saddle area (where you would sit on a bike seat), it’s wise to be evaluated by a spine specialist ASAP.*
How long does it take for a herniated disc to heal?
Conservative treatment healing times vary due to many factors, including the severity of the herniation, presence of other health conditions, compliance with treatment, your occupation, and level of function you’re returning to.
Small herniated discs can heal in as little as 6-8 weeks with proper treatment. Others may take six months to one year to fully recover and return to higher-level exercise, occupational, or sports activities.
Herniated discs are thought to heal via a combination of immune system response, reabsorbing water and other cellular material, and mechanical exercises to relieve pressure on the nerve.
It’s also possible for the pain to subside without the herniation healing. MRIs frequently reveal herniations in asymptomatic people. Could this lead to future flare-ups? It’s possible.
Herniated disc exercises tend to focus on extension because this direction mechanically expands the space and helps relieve pressure off of the spinal nerves.
However, extension exercises may or may not be the best choice for you. It depends.
With multiple conditions, such as spinal stenosis, the position that relieves one can irritate the other. So again, it’s best to work with a physical therapist to find the best rehab program for you.
You can learn more about exercises for herniated discs and back health in the book Treat Your Own Back by Robin McKenzie.
Activities & exercises to avoid with a lumbar herniated disc
While herniated discs can heal on their own, they require that you don’t keep aggravating the area.
If you bite your tongue all day, chances are there will come a time when your tongue hurts even when you’re not biting it. The same concept can be compared to spinal nerves.
If you continue to move in ways that aggravate your pain, by the end of the day you’ll probably have pain no matter what position you’re in. This also makes it difficult to identify pain-free positions and get on the right exercise program.
Friendly PSA – this doesn’t mean “avoid these activities for life.” It just means modify your activities so you can heal and gradually progress back to them.
Here are some everyday activities and exercises that can prolong your rehab.
Complete rest
In very acute phases of injury, you will likely need to take it slow and may need to spend considerable time resting. However, avoiding movement altogether doesn’t fix problems.
Complete rest often prolongs your rehabilitation time and gives a false sense of improvement.
When you start moving again, the pain is right there waiting for you, sometimes even worse than before.
Circulation, blood flow, mobility, and specific controlled movements can help you get better faster.
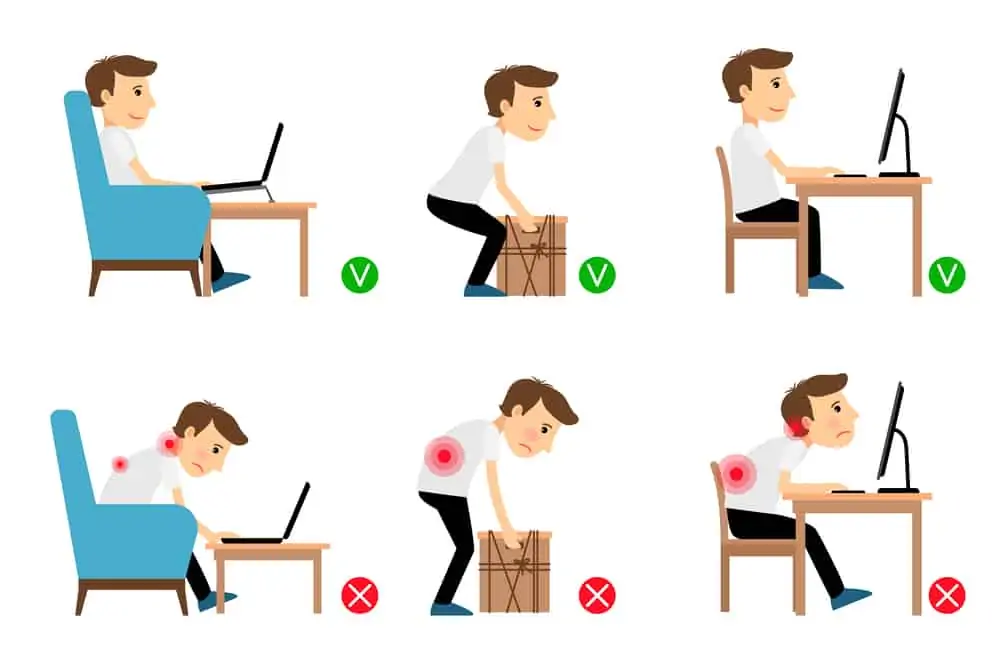
Too much sitting
Sitting, especially in a slouched position, reverses the natural curvature of the lumbar spine. With a herniated disc, this keeps the protruding disc pressing on the spinal nerves.
Too much sitting, including driving, can aggravate disc symptoms.
When you need to sit, use a lumbar cushion to maintain the spine’s natural curvature and take pressure off of the spinal nerves.
There are a lot of choices when it comes to lumbar cushions and lumbar rolls.
The best one is the one that’s comfortable for you.
Some people like a roll like this Original McKenzie roll, and others prefer a more contoured cushion.
You can also use a sit-stand desk to vary your position throughout the day. Switching between standing and sitting every 20-30 minutes can help manage back pain or avoid new onset back pain.
Don’t miss this article analyzing the pros and cons of standing desks.
Too much forward bending
It’s not until you can’t that you realize how much you need to bend during the day.
Forward bending isn’t inherently bad, but it can be very aggravating when you’ve got an angry disc herniation.
Most tasks are in front of our bodies and require a fair amount of bending throughout the day. Unfortunately, forward bending and rounding the spine, such as with gardening, laundry, or yard work, can aggravate your pain.
When you do need to do these activities, bend the knees and hinge from the hip to keep the lumbar spine from excessively rounding and placing more stress on healing tissues.
If possible, use higher surfaces for placing laundry or other tasks. You can also try laundry baskets that are taller and have handles to avoid bending and lifting while you recover, like this one from Amazon.
You can also use adaptive tools like a long handled reacher, long handled shoe horn, and sock-aid to get you through the day. Adaptive tools are especially helpful to maintain independence while not aggravating your pain.
This 7 piece kit has all the tools you need to get you through this frustrating time.
Relying on passive modalities
Passive modalities yield passive results.
These are things like ice packs, hot packs, and tens units. They may provide some temporary pain relief, but they won’t get you where you need to go, just like extensive resting.
These tools absolutely have a place in supplementing your rehab, but the takeaway here is that you won’t suddenly be cured by lying on an ice pack all day.
If these can help take the edge off so you can get moving with the proper exercises, then that’s a win. But you can’t rely solely on passive treatments.
Read more about tens units for pain relief in this article, where I dive deeper into the benefits, risks, and myths.
High impact exercise
Discs absorb shock. High impact exercise translates more force through the body and can aggravate injured tissues.
Activities such as running, HIIT, martial arts, kickboxing, and certain sports, should be avoided to allow your body to heal.
Swap in low-impact workouts to stay moving and avoid prolonging your rehab.
Remember, low impact doesn’t mean low intensity. In this article, I’ll show you 18 low-impact workout alternatives to keep you moving.
Heavy weight lifting
If you’re accustomed to lifting heavy, this compression force through the spine can increase your pain.
Depending on your case, you may be able to continue some strengthening with lighter weights, but this is a conversation between you, your doctor, and physical therapist.
Sit-ups and other abdominal exercises
Sit-ups aren’t even all they’re cracked up to be and one of the worst choices to strengthen your “core.”
They’re especially aggravating to lumbar disc herniations due to the movement pulling you into spinal flexion.
Choose core exercises carefully and avoid ones that involve spinal flexion or twisting until you’re cleared to return to full activity.
Aggressive stretching
The sciatic nerve follows along the back of the leg and can give you the perception of your hamstrings feeling tight.
If the sciatic nerve is irritated, putting tension on the nerve by stretching will most certainly aggravate the pain, like pulling a rope at both ends.
Examples of a hamstring stretch are bending over to touch your toes with straight legs or sitting with your legs out and leaning forward to touch your toes. This also includes downward facing dog.
Use props like The Original Stretch-Out Strap to keep yourself safe and avoid overstretching. This strap has loops along the entire length to ensure you can find the position that’s comfortable for you.
For the low back, extreme rotation or positions to “crack” your own back might further irritate spinal nerves around the herniation.
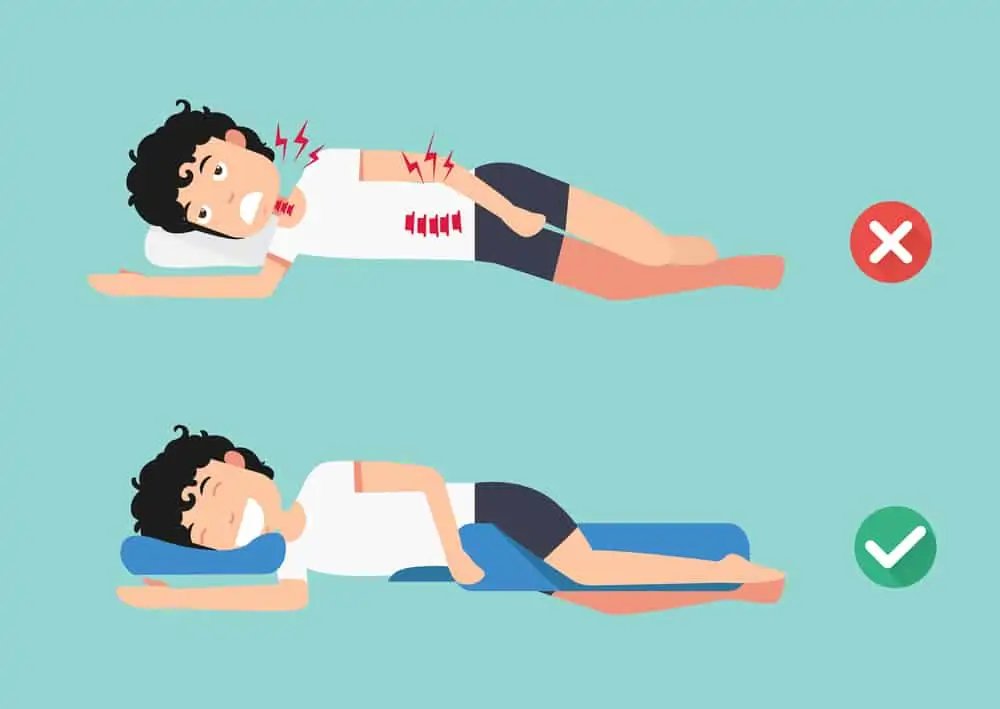
Poor sleeping positions
Sleep disruption is commonly reported with disc herniations.
Studies have predicted there is a reciprocal relationship between sleep and pain. The less quality sleep you get, the harder it is for the body to heal. Round and round we go, deeper into this vicious cycle.
The best sleep position is one that’s comfortable for you while maintaining good alignment of the spine.
For side-sleepers, using a body pillow between the knees helps to support the hips and low back to maintain alignment and avoid extra strain on tissues.
Whether you’re a back or side sleeper, this lumbar pillow is specifically designed to improve alignment to avoid nerve compression while you sleep.
When lying on your back, a wedge to elevate your legs and give a break to the spinal nerves may be a comfortable option. This is also useful for a 20-minute break during the day to relieve inflammation and pain.
Anything that exacerbates your symptoms
Back pain can be tricky and not always follow a textbook presentation and you may need to tweak advice to work for you.
Modify activities or tackle tasks in smaller chunks to avoid flaring up your symptoms constantly.
You’ll heal faster if you can avoid taking one step forward and two steps back.
Tips to get better faster
Here are some helpful proactive steps to take an active role in your rehabilitation and get the proper treatment faster.
- DO get evaluated to determine the cause of your pain and set you up with the proper exercise program for you. The longer you wait on treatment, the longer it can take to get better.
- DO pay attention to your symptoms so you can articulate them to your health care providers to receive a more specific treatment.
- DO learn about your condition so you can better understand safe ways to move and avoid exacerbations.
- DO be consistent with your prescribed home program.
- DO speak up and problem solve with your healthcare providers when something isn’t working.
- DO manage your expectations for healing and celebrate small wins toward getting back to normal.
Wrapping up
A disc injury doesn’t mean you’re going to be limited for the rest of your life. The majority of cases can heal on their own with the proper guidance and treatment.
Remember, a large part of the healing process depends on your ability to find the right ways to move and to be consistent with your program.
Use these tips to avoid exacerbating your pain and get evaluated early to start on the right path to feeling better.
If you’ve never had physical therapy before, don’t miss How To Prepare For Your First Physical Therapy Appointment for all the details before you go.
Send this article to someone who needs to hear these tips!
References
Altun I, Yüksel KZ. Lumbar herniated disc: spontaneous regression. Korean J Pain. 2017;30(1):44-50. doi:10.3344/kjp.2017.30.1.44
Dydyk AM, Ngnitewe Massa R, Mesfin FB. Disc Herniation. [Updated 2021 Jul 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/
Gugliotta M, da Costa BR, Dabis E, et al. Surgical versus conservative treatment for lumbar disc herniation: a prospective cohort study. BMJ Open. 2016;6(12):e012938. Published 2016 Dec 21. doi:10.1136/bmjopen-2016-012938
Inoue N, Espinoza Orías AA. Biomechanics of intervertebral disk degeneration. Orthop Clin North Am. 2011;42(4):487-vii. doi:10.1016/j.ocl.2011.07.001
Morey J. Kolber & William J. Hanney (2009) The dynamic disc model: a systematic review of the literature, Physical Therapy Reviews, 14:3, 181-189, DOI: 10.1179/174328809X452827
Schoenfeld AJ, Weiner BK. Treatment of lumbar disc herniation: Evidence-based practice. Int J Gen Med. 2010;3:209-214. Published 2010 Jul 21. doi:10.2147/ijgm.s12270





Thank you for sharing! I’ve just spent a night back in hospital in A&E because of my back pain – I think I wanted too early too much. So it was a painful lesson of how important it is to listen to our bodies. Although it’s a bit tricky with back pain as you know staying active is good for your back but then you also hear how you should listen to your body…Pushing yourself is good, but not to the breaking point. Healing is a long journey, not a linear one, but I’ll get there, when the time is right.
Thank you, Maura, for this fabulous article! It is extremely informative! I’m going to implement several of your suggestions. I’ve already ordered from Amazon the laundry basket you suggested.
very informative, sharing this also to my brother who got some disc issues because of too much lifting ? I usually do side sleep and having a pillow in between the legs also helps. thanks for this.
I can relate to bad neck/back issues. I have spinal stenosis in the upper part of my neck which makes it hard to turn my head left and right and up and down.