This post may contain affiliate links. If you click through a link and make a purchase, I may receive a commission at no additional cost to you. As an Amazon Associate, I earn from qualifying purchases. Read the full disclosure here.
Here today, gone tomorrow, then back again. The cycle of getting better from things like sciatica can seem up and down like a yo-yo, making it difficult to judge if your sciatica is getting better (or not).
In this article, we’ll discuss three signs that your sciatica is improving that I share with all my patients to help visualize the light at the end of the tunnel.
Disclaimer: This content is for educational purposes and is not medical advice. Read the full disclaimer.
What is sciatica?
To understand how sciatica improves, we need to clarify a bit of background information. Sciatica is often oversimplified, and unfortunately, this contributes to the spread of misinformation.
People are quick to call almost any pain down the back of the leg “sciatica” without further teasing out the details.
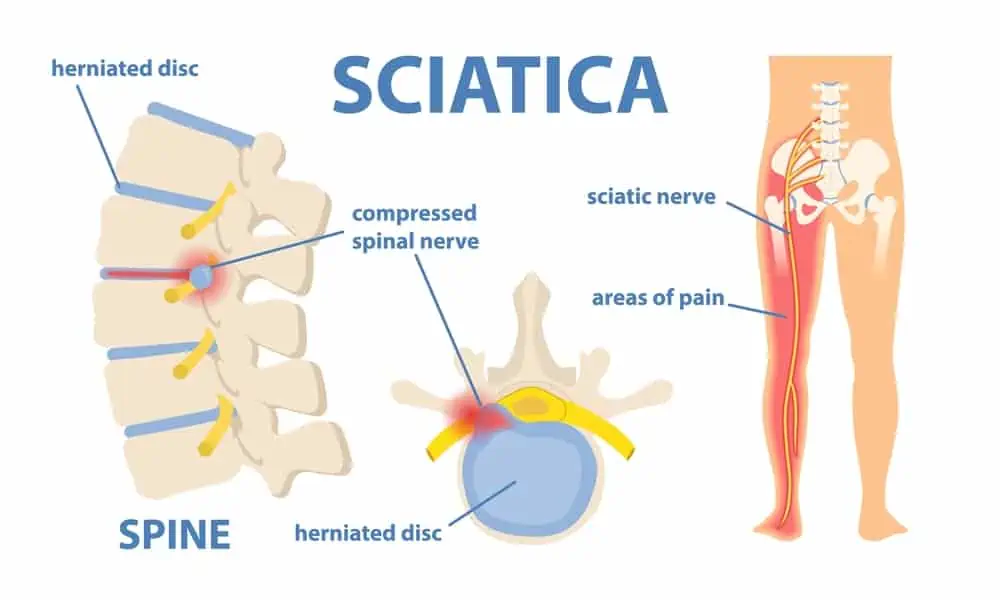
The term sciatica is not a diagnosis but rather a description of a symptom (irritation of the sciatic nerve), and used by itself, is rather vague. Technically, sciatica refers to any irritation of the sciatic nerve along its path (which isn’t very specific).
Many sciatica pain cases originate from the spine, such as with a disc bulge (slipped disc), causing inflammation of the lower spinal nerves (lumbar radiculopathy). This is sometimes referred to as a pinched nerve or sciatic nerve root pain.
However, there are several other ways the sciatic nerve can become inflamed along its path and either cause or mimic sciatic pain. Each of these causes requires a different exercise approach. Therefore, teasing out why you have sciatica is essential in getting the proper exercises to start feeling better.
3 Signs your sciatica is getting better
It can be tricky to notice day-to-day improvement. Here are three key signs to look for as a positive signal that your sciatica is getting better.
You have less pain
Pain is one of the biggest tip-offs that something is wrong. Humans are pretty good at ignoring mild pain, however, when the pain becomes more severe, this can limit quality of life quite a bit.
No one likes the question, “what’s your pain from 1-10?” But it’s actually quite a helpful tool for tracking/monitoring pain. Let me explain.
First of all, you’re not competing with anyone when this question is asked. There’s not some secret leader board that will forever label you as “weak” if you say your pain is a 10.
Everyone’s perception of pain is different, so keep in mind that you’re only tracking against yourself. No one is judging you for the pain level you provide.
Pain is a very individualized experience shaped by many things, including physical, mental, and environmental factors.
So, onto what the pain scale actually interprets to.
Pain level between 1-3
This is considered to be more mild pain or, as some people like to say, “discomfort.”
Pain in this range is more uncomfortable and annoying than truly painful, and you can likely ignore it pretty well and go on with your day.
You’re probably not reaching for over-the-counter meds or ice packs just yet.
Related read: Ice Or Heat For Sciatica?
Pain level between 4-6
This is now the moderate pain range. Pain in this range is more likely to be on your mind throughout the day.
You may consider reaching for some over-the-counter pain medication or cutting back on your activities as your movement tolerance starts to be affected.
This pain is more difficult to ignore and might start to make you irritable. You also might be reaching for the ice pack or heat therapy, or possibly that TENS unit that’s been in the closet.
Related read: Can You Overuse a TENS unit?
Pain level between 7-10
Pain in this range is severe. It may be difficult to concentrate on anything other than pain.
Over-the-counter or even prescription pain medication may be a consideration.
Only a few positions may be comfortable at this point and you may be surviving on ice packs or heat packs to take the edge off of your pain.
There’s a decreased area of radiating pain
The more irritated the sciatic nerve is, the more likely it is for the pain to travel further away from the site of injury. This is called peripheralization.
Some cases of sciatica may produce pain, numbness, or weakness all the way to the foot, while others may stop at the knee or buttock.
Keep track of where your pain extends, and look for signs of centralization, meaning the area of pain is becoming smaller and recedes closer to the spine. During this process, some report an increase in low back pain.
Peripheralization and centralization are terms used to describe the pattern of radiating symptoms when any spinal nerve is compressed. This can occur in the upper or lower body. Sciatica is simply specific to nerve root compression of the sciatic nerve.
Improved tolerance to positions or activities
When your sciatica pain started, you probably noticed some positions or activities increased your pain.
As your pain improves, you’ll hopefully notice an improved tolerance to certain positions or movements.
This may present as either decreased pain, decreased area of pain, or an increased time period before symptoms onset.
You may find you can stretch a little further into a range of motion with less pain. As pain improves, the perception of tight muscles may also lead to some pain relief.
To learn which movements tend to aggravate sciatic pain, read What To Avoid When You Have Sciatica.

When to see a doctor
If you’ve had sciatic nerve pain before, you may be familiar with the pattern and have some exercises in your toolbox to help ease the pain.
If there’s no amount of improvement in 1-2 weeks with your usual plan, it might be time to see a doctor.
Other reasons to see a doctor are:
- A rapid change in sensation, strength, or bowel/bladder function
- Severe pain, the need for pain management
- If you’ve never had this pain before and are unsure what it is
- To get a more specific diagnosis of the root cause of your pain to determine the correct course of treatment
Sciatic pain can arise from a variety of sources, including a herniated disc, spinal stenosis, piriformis syndrome (deep gluteal syndrome), and SI joint dysfunction. Each of these issues requires a different exercise approach.
Symptoms of sciatica
Sciatica symptoms vary in intensity and severity and cases can present very differently between people.
Some common symptoms of sciatica are:
- Moderate to severe lower back pain, back of the hip/buttock, and leg pain
- Sensation changes such as numbness, tingling, pins and needles, or prickly sensations
- Muscle weakness
- Muscle tension/ muscle spasm
- Pain and symptoms can be anywhere along the distribution of the sciatic nerve
If any of these symptoms are accompanied by loss of bowel or bladder function or numbness in the area where you would sit on a saddle, get to the doctor ASAP because that’s a medical emergency.
To read more about what other diagnoses or conditions can cause or mimic sciatic pain, read this article.
How to ease sciatic pain
One of the best strategies to begin to ease your sciatic pain is to determine which movements/positions make the pain feel better and which make it feel worse.
Read this article, What To Avoid When You Have Sciatica, to learn some of the most common things that make sciatica pain worse.
Wrapping Up
Sciatica can be frustrating and painful. Look for these signs of sciatica improving to help gauge where you are in the recovery process.
Don’t hesitate to reach out to your doctor or physical therapist for guidance. Getting symptoms addressed early can help you avoid chronic pain in the future.
References
Davis D, Maini K, Vasudevan A. Sciatica. [Updated 2020 Nov 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507908/
Visser LH, Nijssen PG, Tijssen CC, van Middendorp JJ, Schieving J. Sciatica-like symptoms and the sacroiliac joint: clinical features and differential diagnosis. Eur Spine J. 2013;22(7):1657-1664. doi:10.1007/s00586-013-2660-5
Thiyagarajan, Senthilkumar. (2017). Pseudo Sciatica-It’s the Condition we really Treat Better than Medicine. Journal of Novel Physiotherapies. Volume 7. 10.4172/2165-7025.1000327.